Introduction
Infectious disease diagnostics have evolved rapidly in recent years, driven by advancements in technology and a growing need for quicker, more accurate detection methods. New innovations are transforming the diagnostic landscape, making it possible to identify infections with unprecedented speed and precision. From molecular diagnostics to AI-driven tools, these advancements are helping healthcare providers respond to infectious threats more effectively. In this article, we will explore the latest innovations in infectious testing, shedding light on how they are enhancing our ability to manage public health.
Definition
Infectious testing refers to the range of diagnostic procedures and tools used to detect the presence of infectious agents, such as bacteria, viruses, fungi, and parasites, within a host organism. This type of testing is crucial in identifying diseases that can spread from one individual to another, enabling healthcare providers to diagnose infections early, determine appropriate treatment plans, and implement measures to prevent further transmission. Infectious testing methods vary widely and include molecular techniques like PCR, antigen and antibody detection, culture tests, and rapid point-of-care tests, each designed to provide accurate and timely identification of pathogens responsible for infectious diseases.
Molecular Diagnostics: A New Standard in Speed and Accuracy
Molecular diagnostics have become a cornerstone in infectious disease testing, offering unmatched accuracy in detecting pathogens. Techniques such as polymerase chain reaction (PCR) and next-generation sequencing (NGS) are widely used to analyze DNA or RNA from pathogens, providing insights into their genetic makeup. These tests are highly sensitive, often able to detect infections even before symptoms appear.
Isothermal Amplification Technologies: Unlike PCR, which requires temperature cycling, isothermal amplification can rapidly amplify DNA at a constant temperature. Techniques like Loop-Mediated Isothermal Amplification (LAMP) enable faster results, making them ideal for point-of-care (POC) testing in settings with limited resources.
CRISPR-Based Diagnostics: Clustered Regularly Interspaced Short Palindromic Repeats (CRISPR) technology is being adapted for diagnostic purposes. CRISPR-based tests can target specific genetic sequences associated with pathogens, making them useful for detecting various infections, including viral, bacterial, and parasitic diseases. CRISPR diagnostics are not only fast but also highly accurate, marking a significant leap forward for rapid testing in the field.
Point-of-Care (POC) Testing: Increasing Accessibility and Reducing Time to Diagnosis
Point-of-care testing has gained prominence, particularly in rural and remote areas where access to centralized labs can be limited. POC testing devices allow healthcare providers to perform tests directly at the patient’s location, providing results within minutes to hours rather than days.
Microfluidics and Lab-on-a-Chip (LOC) Devices: Microfluidic devices have miniaturized lab procedures, fitting entire diagnostic processes onto a single chip. LOC devices can analyze blood, saliva, or other samples with minimal input, delivering results in a fraction of the time needed for conventional lab tests. With their portability, these devices are proving invaluable in managing infectious outbreaks and improving care in underserved regions.
Biosensors and Wearable Devices: Recent advances have introduced biosensors and wearable devices capable of continuously monitoring for signs of infection. These devices detect biomarkers that indicate the presence of pathogens, allowing for real-time monitoring of patient health and potentially catching infections in their early stages.
Rapid Antigen and Antibody Tests: Revolutionizing Infectious Disease Control
Rapid antigen and antibody tests have reshaped the approach to infectious disease control, especially for illnesses like COVID-19, influenza, and hepatitis. These tests detect specific proteins or antibodies produced in response to an infection and can deliver results in minutes, aiding in mass screenings and rapid response efforts.
Lateral Flow Assays (LFAs): LFAs are commonly used for rapid antigen and antibody testing due to their simplicity and low cost. These strip-based tests can identify viral proteins in nasal or saliva samples with high specificity. They are particularly useful in large-scale screening efforts and can be administered by non-specialists, making them a popular choice for community-based testing.
Electrochemical Biosensors: Unlike traditional antigen and antibody tests, electrochemical biosensors use electrodes to detect pathogens at the molecular level. These sensors provide quantitative data, increasing their accuracy and making them suitable for applications requiring precise measurements. Their low cost and compact design have made them an attractive option for mass diagnostics.
Artificial Intelligence (AI) and Machine Learning: Enhancing Diagnostic Precision
AI and machine learning have introduced a new dimension to infectious disease diagnostics, enabling faster analysis of large datasets and improving the accuracy of diagnostic tests. These technologies are particularly effective in identifying patterns that human eyes might miss, allowing for quicker and more accurate diagnoses.
AI-Enhanced Image Analysis: AI algorithms are now used to analyze images from blood smears, x-rays, and other medical imaging to detect infectious diseases like tuberculosis and malaria. Machine learning models can differentiate between healthy and infected cells with high accuracy, enabling faster diagnosis in resource-limited settings where trained specialists may be scarce.
Predictive Analytics for Outbreak Detection: AI-based predictive analytics can track infection trends and predict outbreaks. By analyzing patient data and environmental factors, these models can provide early warnings of emerging infectious diseases, helping healthcare systems prepare and respond more effectively.
Digital PCR (dPCR) and Quantitative PCR (qPCR): Improved Sensitivity for Low-Level Infections
Digital PCR (dPCR) and quantitative PCR (qPCR) have improved the ability to detect pathogens at very low concentrations, which is essential for diagnosing infections in their early stages or identifying carriers with asymptomatic infections.
dPCR in Viral Load Testing: Digital PCR divides a sample into thousands of tiny droplets, allowing for precise counting of DNA molecules within each droplet. This technique is especially useful for viral load testing in conditions like HIV and hepatitis, where tracking the amount of virus in the blood can guide treatment plans and assess disease progression.
qPCR for Quantifying Pathogen Levels: Quantitative PCR is widely used for determining pathogen levels, especially in monitoring antibiotic resistance genes and pathogen load in clinical samples. Its sensitivity makes it ideal for assessing treatment efficacy and tracking the spread of infectious agents within populations.
Multiplex Testing: Detecting Multiple Pathogens in a Single Test
Multiplex testing allows healthcare providers to screen for multiple pathogens simultaneously, significantly reducing the time needed for diagnosis. This is particularly useful in cases where symptoms are non-specific and could indicate a range of potential infections.
Multiplex PCR Panels: Multiplex PCR can identify several pathogens in a single test, saving valuable time in cases where rapid diagnosis is critical. This method is increasingly used for respiratory infections, gastrointestinal diseases, and sexually transmitted infections, allowing for comprehensive diagnostic coverage in one go.
Syndromic Testing Platforms: These platforms group pathogens based on the symptoms they cause, offering quick and reliable results for conditions such as fever of unknown origin. Syndromic testing is especially useful in emergency settings where identifying the causative pathogen can lead to timely treatment.
Whole Genome Sequencing (WGS): Tracing Pathogens with Precision
Whole genome sequencing has transformed pathogen detection by providing a complete genetic map of infectious agents. WGS is not only useful in identifying infections but also in understanding how they evolve and spread, making it a valuable tool in public health surveillance.
Tracking Antibiotic Resistance: WGS can reveal mutations linked to antibiotic resistance, helping to guide appropriate treatment. By comparing genetic sequences, researchers can also track the spread of resistant strains and implement targeted interventions.
Epidemiological Surveillance: During outbreaks, WGS can trace the source and spread of pathogens, providing valuable data for controlling disease transmission. This has been particularly valuable in tracking COVID-19 variants, allowing for a better understanding of how mutations impact transmissibility and vaccine efficacy.
Cloud-Based Data Sharing and Telemedicine Integration: Enabling Faster, Coordinated Responses
Infectious disease diagnostics are increasingly linked to cloud-based data sharing platforms that allow healthcare providers to access and share diagnostic data in real time. This integration facilitates quicker responses to infectious outbreaks by enabling seamless communication across healthcare systems.
Telemedicine Integration: Many diagnostic tools are now integrated with telemedicine platforms, allowing patients to get tested remotely and receive results virtually. This is particularly advantageous for those in remote locations, as it minimizes travel and reduces the potential spread of infectious diseases.
Global Health Surveillance Networks: Cloud-based platforms enable health organizations to share real-time data on emerging infections, aiding global health surveillance and response efforts. By quickly identifying and tracking potential outbreaks, these networks help prevent the spread of infectious diseases on an international scale.
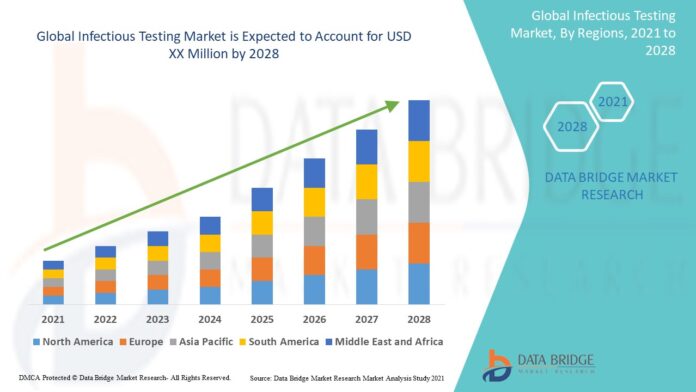
Growth Rate of Infectious Testing Market
Data Bridge Market Research forecasts that the infection testing market will grow at a CAGR of about 4.82% between 2021 and 2028.
To read more click here.
https://www.databridgemarketresearch.com/reports/global-infectious-testing-market
Conclusion
The innovations in infectious testing are revolutionizing how we diagnose and respond to infectious diseases. As these technologies continue to evolve, they promise to enhance diagnostic precision, reduce time to diagnosis, and make testing more accessible than ever. From molecular diagnostics to AI-driven image analysis and cloud-based data sharing, these advances are transforming the landscape of infectious disease diagnostics, offering hope for a future where infectious threats can be swiftly identified and contained.